
Have you caught those sideways glances that happen when someone coughs or sniffles in public? In years past, we’d often chalk up common symptoms like fatigue, congestion and a runny nose to an illness that would pass with chicken noodle soup and a few days on the couch. This year, the stakes are higher.
Exposure to COVID-19 doesn’t just mean missed days of work and quarantining the kids at home away from classmates. It can also result in severe illness, hospitalization and families who are mourning losses and have empty chairs around the table at the holidays.
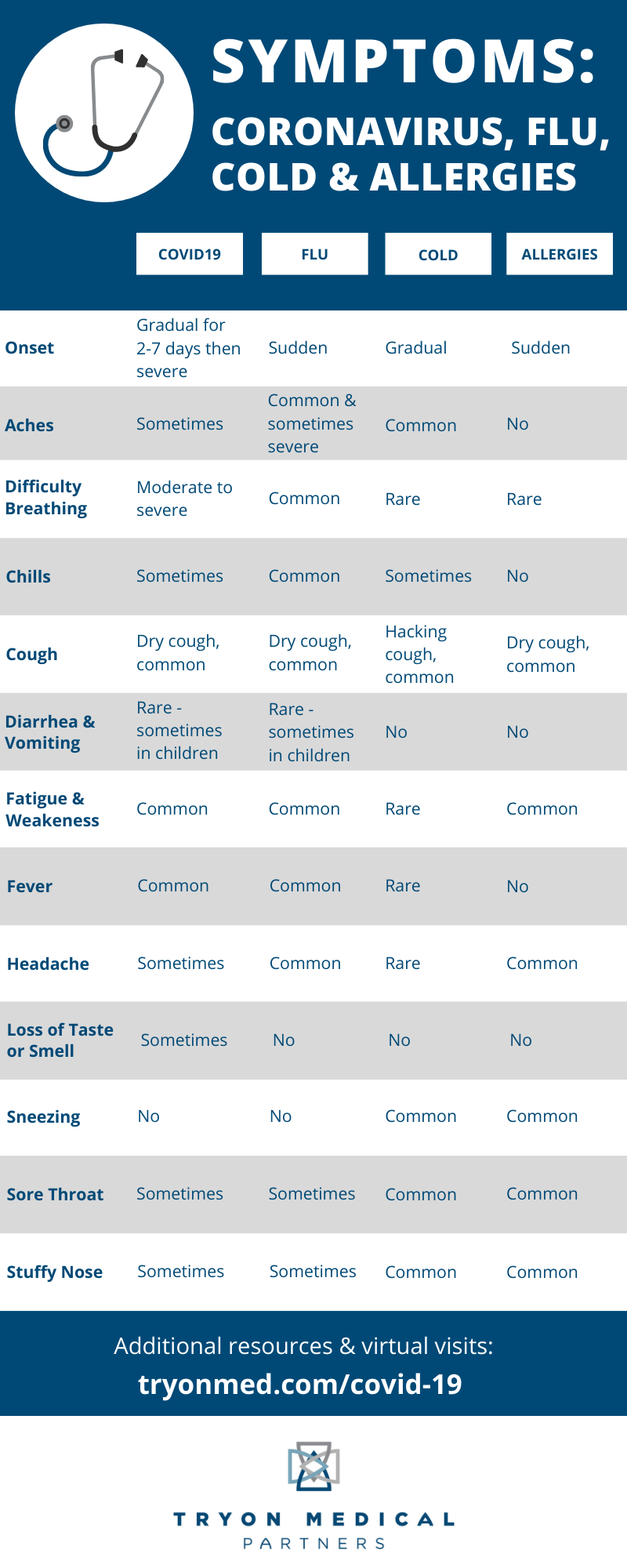
With so many crossover symptoms between COVID-19, flu, colds and allergies, we can rightfully be a bit leery of a cough or sore throat. Now in the midst of flu season and during the winter when activities move indoors, it’s important to know your symptoms.
The doctors at Tryon Medical Partners have been on the front lines of COVID-19 from the beginning. Just days after the first positive case in Charlotte, they opened satellite clinics for testing and spearheaded research locally that resulted in the COVID-19 vaccines we rely on today.
With all this experience evaluating symptoms and caring for patients, the doctors at Tryon share more about how to manage symptoms when they occur in your own family.
 Is it COVID-19 or the flu?
Is it COVID-19 or the flu?
COVID-19 and the flu are both respiratory illnesses, but they are caused by different viruses. Similarly, both can cause severe illness or result in an asymptomatic status, meaning a person is infected but shows no symptoms. Both illnesses can result in fever, cough, fatigue, headaches, muscle and body aches, and a runny nose or congestion.
The key distinguisher of the flu is its sudden onset and body aches. When associated with COVID-19, symptoms often come on more gradually.
Vaccinated patients who have breakthrough COVID-19 may have very mild symptoms that seem like a run-of-the-mill cold or sinus infection.
Knowing when to get tested
Since breakthrough COVID-19 cases can present with more moderate symptoms, getting tested is key.
“While the prevalence of COVID-19 in the community is relatively high, patients should consider getting a test even if their symptoms seem compatible with just a cold or the flu,” says Dr. Jennifer Womack, an internal medicine specialist at Tryon Medical Partners Uptown.
If you or a loved one are experiencing COVID-19 symptoms, the first reaction is often to want to test immediately using the method that returns the fastest results. But by following this logic, you may be risking the sensitivity and, thus, the accuracy of the test.
“When done too early, COVID-19 testing can result in a false-negative,” Dr. Womack says. “The virus, if present in your body, is still in the process of multiplying and may not be at high enough numbers to show on a test yet.”
Tests are the most sensitive after 72 hours of symptoms. If you have tested earlier than 72 hours after symptoms began and received a negative result, stay home, mask up and complete another test after three days of symptoms. If you’ve been exposed to COVID-19, your best testing time frame depends on your vaccination status and how you’ve been exposed.
Staying well through prevention
While the root of your symptoms may not always be clear without consulting your physician, the good news is that we have vaccines for COVID-19 and the flu. The best way to prevent getting sick with either is to get your vaccine and booster dose.
The techniques we’ve been practicing to prevent COVID-19 should still be in your playbook. Wash your hands, stay socially distant and wear a mask. These also work to prevent other respiratory illnesses like flu and colds.
“I recognize that many people are feeling ‘COVID fatigue,’ but with new variants emerging like Omicron, we really need to dial up our due diligence,” says Dr. Ryan Shelton. “It’s time to double down on the basics, including mask-wearing, social distancing and avoiding large gatherings.”
COVID-19 vs. cold and allergies
Like COVID-19 and the flu, a common cold is also caused by a respiratory virus, most often the rhinovirus, known to trigger asthma attacks and sinus and ear infections. Colds result in symptoms that are often far less severe than COVID-19, cause relatively minor complications and are likely to go away on their own.
With a cold, you are less likely to have a fever and the symptoms that accompany fever, like chills, fatigue, weakness and body aches. A sore throat and runny nose are most common in the early onset of a cold.
In winter months, seasonal allergies are not common and most allergies at this time of year stem from indoor mold. Allergies have a sudden onset, while symptoms of COVID-19 present more gradually. Fever does not accompany allergies, nor do fever-related symptoms. Allergy sufferers are most likely to find themselves with headaches, sneezing, sore throat, stuffy nose and a dry cough.
Despite all the uncertainty of common symptoms between COVID-19, flu, colds and allergies, you can rest easier and make the best choices for your family when you have a trusted physician on your side. Be sure not to put off the everyday care you need in order to stay healthy and, if you’re worried about any symptoms, schedule an appointment with your doctor and get tested.


